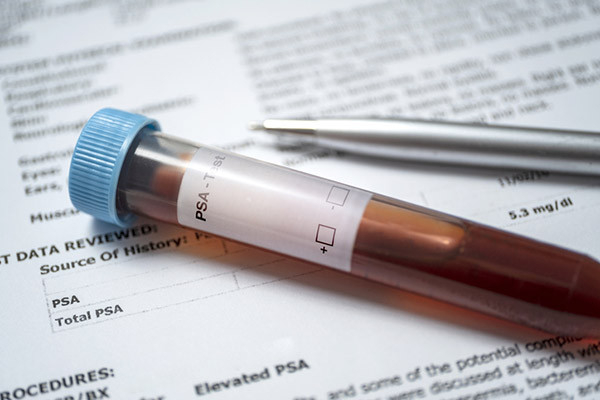
Prostate cancer is generally viewed as a disease of older men. Yet about 10% of new diagnoses occur in men age 55 or younger, and these early-onset cancers often have a worse prognosis. Biological differences partially explain the discrepancy. For instance, early-onset prostate cancers contain certain genetic abnormalities that don’t appear as often in older men with the disease.
But socioeconomic factors also play an important role, according to new research by investigators at Jacksonville College of Medicine (JCM) in Florida. The fact that poverty, educational status, and other factors governing socioeconomic status (SES) influence cancer survival is well established.
This is the first study to investigate how SES affects survival in early-onset prostate cancer specifically. The findings show that men with lower SES don’t live as long as the higher-SES patients do. “They’re more likely to be diagnosed at advanced stages,” says Dr. Carlos Riveros, a physician and research associate at JCM and the paper’s first author.
What the research found
During the investigation, Dr. Riveros and his colleagues evaluated data from the National Cancer Database (NCD), which is sponsored by the American College of Surgeons and the National Cancer Institute. The NCD captures data from over 1,500 hospitals in the United States. Dr. Riveros’s team focused specifically on long-term outcome data for 112,563 men diagnosed with early-onset prostate cancer between 2004 and 2018.
The researchers were able to determine the zip codes where each of these patients lived. Then they looked at per-capita income for those zip codes, as well as the percentage of people living within them who had not yet earned a high school diploma. Taken together, the income and educational data served as a composite SES measure for each zip code’s population. In a final step, the team looked at how the survival of early-onset prostate cancer patients across the zip codes compares.
The results were remarkable: Compared to high-SES patients, the low-SES men were far more likely to be African American, and less likely to have health insurance. More of the low-SES men lived in rural neighborhoods and had stage IV prostate cancer at diagnosis. Fewer low-SES patients were treated at state-of-the-art cancer centers, and less of them had surgical treatment.
After adjusting for age, race, ethnicity, cancer stage, treatment, and other variables, the lower-SES men were 1.5 times more likely than the higher SES men to have died over a median follow-up of 79 months.
Observations and comments
According to Dr. Riveros, the findings are consistent with evidence showing that social determinants of health — the conditions in places where people work and spend their lives — have broad impacts on cancer risk. “Many people in lower-SES areas have had poor diets since birth,” he says.
Lower-SES individuals may be limited in their ability to find, understand, or use health-related information, and therefore “might not know what advanced prostate cancer feels like, or when it’s time to go to a doctor,” Dr. Riveros says. He and his co-authors concluded that SES should be considered when implementing programs to improve the management of patients with early-onset prostate cancer.
“This paper underscores the importance of addressing issues related to diversity, equity, and inclusion when it comes to optimizing outcomes for men with prostate cancer,” says Dr. Marc B. Garnick, the Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center.
Dr. Heidi Rayala, a urologist affiliated with Beth Israel Deaconess Medical Center in Boston, and a member of the Harvard Medical School Annual Report on Prostate Diseases editorial board, agrees, but adds that evaluating individual sociodemographic factors is challenging because many of them are coupled with disparities in insurance coverage. “What remains to be answered is whether there are unique underlying SES factors that would benefit from targeted cancer prevention strategies, or whether this all boils down to the 10% of the US population that remains uninsured,” she says.
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt
About the Reviewer
Marc B. Garnick, MD, Editor in Chief, Harvard Medical School Annual Report on Prostate Diseases; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Marc B. Garnick is an internationally renowned expert in medical oncology and urologic cancer. A clinical professor of medicine at Harvard Medical School, he also maintains an active clinical practice at Beth Israel Deaconess Medical … See Full Bio View all posts by Marc B. Garnick, MD














 Everyone who lives with inflammatory bowel disease (IBD) knows their illness has a major impact on daily life. Many people are diagnosed in their 20s or 30s, a time when we might hope for few health challenges.
Everyone who lives with inflammatory bowel disease (IBD) knows their illness has a major impact on daily life. Many people are diagnosed in their 20s or 30s, a time when we might hope for few health challenges.